Introduction
The U.S. Department of Veterans Affairs (VA) has made significant investments in facilities and human capital in the last several years to improve healthcare access for veterans. Although much ground has been gained, veterans’ access to primary care appointments remains a challenge. A primary contributor to the access challenge is primary care provider (PCP) turnover, mostly due to increasing provider burnout and loss of an acceptable work/life balance.
In the private sector, physician turnover rate has averaged 6-8% over the last decade.i Over this same period, our experience working with VA primary care providers (both VA employed and Contractor employed) has demonstrated a PCP turnover rate as high as 19-20%. When considering the required investments in recruitment, relocation, credentialing and privileging, training, and start-up, the costs in both time and money are significant, but the more important cost is the missed opportunity to serve veterans on a timely basis.
One proven and effective tool to improve PCP retention, increase primary care appointment access, and enhance the customer service experience for veterans is the use of medical scribes. This white paper outlines the successful deployment of medical scribes in VA Community Based Outpatient Clinics (CBOCs) operated by Valor Healthcare, the largest provider of contract CBOC services to the VA.
Problem Definition
The VA’s electronic health record (EHR), VistA Computerized Patient Record System (CPRS), is a robust tool that has stood the test of time. However, through the years the administrative burden associated with quality documentation in CPRS has increased considerably for primary care providers. The impact has been significant and multifaceted. Medical providers and veterans alike are dissatisfied with the amount of time providers are required to spend in front of the computer to complete appropriate and accurate medical record documentation. Despite the many merits of EHR systems, physicians and mid-level providers are on record saying they want to take care of patients – not serve as data entry clerks. Yet, as seen in Figure 1, in a typical 30-minute appointment, CBOC medical providers spend an average of seven minutes with the patient.ii The remainder of the appointment time (77%) is spent with the highly trained, highly compensated medical professional completing clerical tasks. Private practice internists typically see 18-20 patients per day and family physicians are used to seeing 25-35 patients per day. For a variety of reasons, PCPs in the VA system generally see 8-15 patients daily. VA patients tend to be older (over half of veterans enrolled in VA healthcare are 65 or older) with longer problem lists and more complex diagnoses. Veterans also have unique health care needs relative to age-matched non-veteran patients.iii
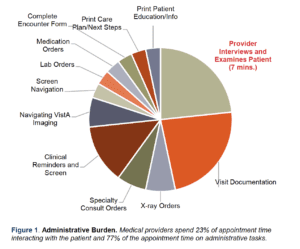
As referenced in Figure 1, after interviewing and examining the patient the PCP is responsible for documenting the progress note for the encounter, ordering medications, labs and/or x-rays, and filling out specialty consult requests. It is also true that, over time, national clinical practice guidelines have resulted in more and more Clinical Reminders being added to CPRS. Many health screens and Clinical Reminders have multiple expanding options embedded in the software
that must be addressed.
While some Clinical Reminders can be completed by nursing staff, many/most of these Clinical Reminders require direct action/input from the provider. At best, the patient sits idly while the provider completes all the administrative documentation. At worst, the provider has his/her back turned to the patient to work on the computer and is completely disengaged from the patient – an experience well-documented and loathed by patients and medical providers alike.
This is not the “veteran-centric, world class customer service experience” former Secretary of the VA Bob McDonald appropriately called for in all VA facilities. It is not what medical providers want to spend their time doing, nor is it the patient/provider experience veterans deserve.
Medical providers have long been attracted to working in the VA system because when working in outpatient clinics, there are no on-call responsibilities and there are no expectations to work nights or weekends. Unfortunately, this is no longer true. Despite seeing only 8- 15 patients per day (depending on clinical experience and computer skills), most PCPs working in VA clinics are no longer able to complete their administrative work (reviewing lab/x-ray reports, returning phone messages, etc.) during normal business hours.
More and more, PCPs must come in early, work through lunch, stay late, and/or request remote access to work on administrative tasks nights and weekends. Tasks that historically were accomplished in between patients must now be deferred to time outside normal business hours because the time “between patients” no longer exists. The ever-increasing administrative burden inherent in working with CPRS simply takes too long, and most of the administrative work being required of physicians, nurse practitioners (NP), and physician assistants (PA) could, and should, be done by someone else on the care team.
There are a number of potential solutions to the challenge described above, and the problem is certainly on the VA’s priority list. In a February 10, 2017 article in Modern Healthcare, a dialogue is described between Rep. Phil Roe, Chairman of the House Veterans Affairs Committee, and Laverne Council, former Assistant Secretary for Information and Technology at VA, discussing whether “the department could retain VistA as its electronic health record system, but purchase commercial-off-the-shelf software, such as customer relationship management software, to perform nonmedical administrative functions that have been incorporated into VistA over the years.”iv
Whether VA bolsters VistA or invests billions in a new commercial EHR, as Military Health Systems did, implementation is not imminent. Valor Healthcare has demonstrated that the use of medical scribes in CBOCs positively impacts the veteran customer experience, primary care appointment availability, and medical provider job satisfaction and retention. This solution can be operational in a matter of weeks in every VA CBOC in the country.
Solution
Industry Best Practices
Examples of private industry best practices of the impact of medical scribes abound. In 2013, Dr. Christine Sinsky, in the Annals of Family Medicine, identified the use of medical scribes as one of the five most effective innovations being used in 23 highly functioning primary care practices.v Likewise, at The Cleveland Clinic – Strongsville, use of a medical scribe resulted in a 38% average increase in capacity along with improved patient and provider satisfaction scores.
The key function of the medical scribe is to accurately capture and document in the EHR detailed patient information in a timely manner (Cambel, Case, & Crocker, 2012). Specifically, the medical scribe:
- Assists the provider with navigating the EHR.
- Enters information in the EHR as directed by the provider.
- Locates information in the EHR that requires review.
- Researches information requested by the provider.
- Responds to various messages as directed by the provider.
VA Momentum
More importantly, the concept of using medical scribes in VA’s integrated healthcare system is not new either. In fact, it has gained considerable momentum in the last 36 months. In July 2014, a VA white paper detailing the benefits of Health Advocates, whose duties include scribing, was presented to VA Principle Deputy Under Secretary for Health Dr. James Tuchschmidt (Schectman, Morgan, & Mancari, 2014). This paper, written by VA proponents for medical scribes, details numerous benefits that include:
- Enhanced veteran-centric care, as the PCP is able to focus solely on the veteran instead of the computer – a common patient complaint in both VA and non-VA outpatient clinic settings.
- Increased appointment access, as the administrative work is shared with the scribe. The PCP focuses on actions that requires his/her higher level of education and training (assessment, diagnosis, treatment plan) while most other actions are performed by other members of the care team.
- Improved PCP job satisfaction and retention, because they feel they are practicing medicine more and performing data entry less. Many PCPs report frustration with inability to complete their administrative work within normal business hours, requiring them to come in early, stay late, or take work home, creating an unacceptable and unsustainable work-life balance.
- Improved recruiting of difficult-to-fill PCP vacancies.
On October 7, 2015, then Secretary of Veterans Affairs Bob McDonald testified before the House Veterans Affairs Committee on a broad range of issues.vi A significant portion of the discussion focused on the use of medical scribes to assist physicians when treating patients. Rep. Phil Roe, MD made an impassioned plea for a scribe pilot in CBOCs in his district, and Secretary McDonald testified that the VA was in fact already piloting programs using scribes.
Regulatory Considerations
The use of medical scribes is supported by The Joint Commission (TJC), and there are detailed TJC guidelines for implementing such a program. Important aspects of TJC guidelines include:
- Identifiable and distinguishable scribe signing/dating.
- Provider authentication of entry via the EHR (CPRS in this case) before provider and scribe leave the exam room.
- Orders, if permitted by the institution, cannot be acted on until authentication by the provider
- Policies/procedures should be in place to ensure the scribe is not acting outside his/her scope of practice or job description.
- Authentication is occurring.
- No orders are acted on prior to authentication.
Valor Healthcare’s CBOC Scribe Program
veterans in our CBOCs. We are second only to the VA itself in the delivery of primary care services to veterans. In 2015-2016, Valor
conducted a pilot in several of our CBOCs in Indiana, Ohio, and Texas. In April 2016, we presented our findings at the Annual Meeting of the American Association of Physician Leaders. Please refer to page 10 to see our poster presentation, Provider’s Best Friend: Impact of a Medical Scribe on Patient and Provider Satisfaction in VA Community Based Outpatient Clinics.
Scribe Program Objectives
- Enhance veteran and provider satisfaction through implementation of a medical scribe program.
- Decrease medical provider turnover and improve veteran access by improving provider efficiency.
- Further VA’s goal for a more veteran-centric, team-based approach to care.
Scribe Program Summary
With the advent of electronic health records and the ongoing clinical need for comprehensive, quality documentation, the amount of time uninterrupted by documentation requirements that medical providers spend in face-to-face interaction with their patients has decreased significantly. This phenomenon can be magnified in the VA healthcare system, specifically in VA Community Based Outpatient Clinics, where additional system-specific documentation requirements further impact the quality of the patient-provider interaction. Our scribe program is designed and implemented with the intent of assisting providers with progress note documentation by minimizing data entry by the provider. The aim is to improve both patient and provider satisfaction with the visit, increase provider face-to-face time with the patient, and potentially save time with each visit without compromising clinical quality or complete and accurate documentation of the visit.
The program utilizes a Licensed Practical Nurse (LPN) as the scribe for the provider because in most VA Medical Centers an appropriately trained LPN can not only document the progress note, but is also authorized to place orders in CPRS (and hold for provider signature) for consults, labs, medications, etc. The LPN utilizes the provider’s documentation template in order to ensure complete documentation in the appropriate SOAP (Subjective/Objective/Assessment/Plan) note format. The provider may optionally utilize a second workstation (laptop computer) in the exam room to review labs and medications with the patient as well as to review the note and orders prior to signature. Whether the provider and scribe utilize one workstation or two, the provider can make any appropriate changes to the note before leaving the exam room, and by the end of the visit all tasks associated with the veteran encounter are complete. This ensures timely and accurate documentation in the electronic health record, and our experience and data demonstrate improved provider Total Time in Room (TTIR) and Provider–Patient Face-to-Face Time (F2F).
Summarized below are the results of our medical scribe pilot. As depicted, we tested our theory on the benefits of scribes with providers who were already experienced with VA’s EHR as well as those who had only recently begun using CPRS.
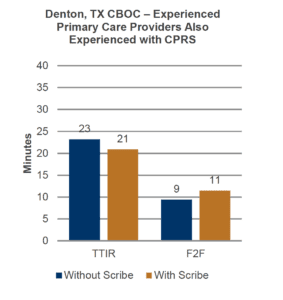
-
10% decrease (2 minutes/visit) in TTIR and a 21% increase (2 minutes/visit) of patient-provider F2F time
-
Two workstations in the room
- At an average of 8 patients/day, using a scribe created 16 minutes in the provider’s schedule that could be used for:
- Administrative time (reviewing labs, returning patient phone calls, etc.)
- 1 additional patient appointment slot per day per provider
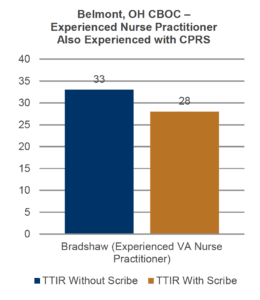
- 15% decrease (5 minutes/visit) in TTIR for this experienced Nurse Practitioner also experienced with VA’s EHR
- Single workstation in exam room
- At an average of 8 patients/day, using a scribe created 40 minutes in the
provider’s schedule that could be used for:- Administrative time (reviewing labs, returning patient phone calls, etc.)
- 1-2 additional patient appointment slots per day per provider
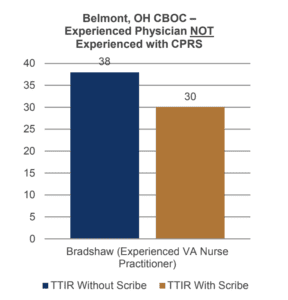
- 21% decrease (8 minutes/visit) in TTIR for this experienced physician new to VA’s EHR
- Single workstation in exam room
- At an average of 8 patients/day, using a scribe created 64 minutes in the provider’s schedule that could be used for:
- Administrative time (reviewing labs, returning patient phone calls, etc.)
- 2-3 additional patient appointment slots per day per day
Scribe Program Benefits
Use of medical scribes in VA CBOCs:
- Decreases Total Time in Room by an average of five (5) minutes per patient and creates 1-3 additional patient appointment slots per day per provider, thus increasing clinic access for veterans
- Increases veteran-provider Face-to-Face Time by 21%. This creates a higher quality visit and a distinctly more veteran-centric healthcare experience
- Increases veteran satisfaction*
- Increases provider satisfaction, leading to reduced provider turnover and enhanced continuity of care for veterans*
Return on Investment (ROI) – Financial
It is important to revisit our use of LPNs to serve as scribes. VA now almost universally employs the Patient Aligned Care Team (PACT) model in its outpatient clinics. The PACT model is VA’s version of the Patient Centered Medical Home model used extensively in private sector primary care. PACT teams are comprised of:
- Primary Care Provider (Physician, NP, PA)
- RN Care Coordinator
- LPN/LVN
- Medical/Administrative Assistant
As mentioned previously, we elected to use the PACT team LPN as the provider’s scribe because, depending on individual VA Medical Center bylaws, an LPN’s scope of practice generally permits him/her to be of maximum value to the provider relative to the tasks he/she can perform in the exam room on behalf of the medical provider. But we must consider that prior to designating the LPN as scribe, he/she was already performing the work required of a PACT team LPN, i.e. rooming patients, doing intake, addressing nursing Clinical Reminders, giving injections, performing ECGs, etc. What happens to all of this workload when the LPN is spending the majority of the workday in the exam room scribing for the provider? Clearly it doesn’t just go away.
In Valor’s scribe model, we employ an additional 0.5 FTE LPN per PACT team to assume the workload no longer being accomplished by the LPN who is now scribing. So an additional LPN for every two PACT teams is required to address calls, messages, lab results, injections, ECGs, etc. Our ROI calculations make certain assumptions based on PACT staffing, provider panel sizes, clinic space, and the level of PACT model implementation at the CBOC.
Assume that a PACT team is assigned a panel of 1,200 veterans and is staffed with a Physician, RN Care Coordinator, LPN, and Administrative Assistant. Furthermore, assume the following annual labor rates (including benefits):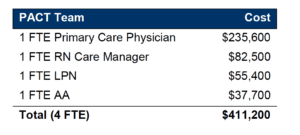
Applying the total labor costs for the PACT team to the number of patients (1,200 in this example) on an assigned provider panel, we estimate that the treatment cost per veteran is $342.67 per year in the standard PACT model with no scribe function.
In contrast, when integrating a scribe into the care team/PACT team, and thus requiring an additional 0.5 FTE LPN per PACT team, assume the following annual labor rates (including benefits):
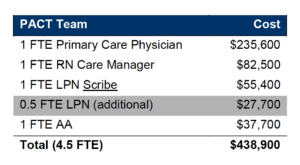
In this model, there is an increased capacity for veterans’ access (demonstrated in the graphs above), which can be applied to provider panel size. Due to the efficiencies and appointment slots gained through use of a medical scribe, we estimate that a provider panel size can be increased by 7% (1,281 veterans in this example). Applying the total labor costs for the PACT team to the minimally increased number of patients on an assigned provider panel, the treatment cost per veteran in this scribe model remains $342.62 per year.
As represented above, implementation of a medical scribe model in VA CBOCs results in a budget neutral effect on the cost per veteran.
Return on Investment (ROI) – Access, Retention, and Continuity
Although more difficult to assign a dollar value, we have demonstrated that implementing a medical scribe program creates provider capacity in terms of veteran access to timely appointments. An additional 1-3 veteran appointment slots per provider per day is clearly material in an environment where veterans’ dissatisfaction around the country continues to focus on access.
Additionally, provider burnout and turnover, along with the resultant impact on access, remains a major hurdle for outpatient clinics operated by VA and contractors alike. PCP turnover in the private sector is estimated to be approximately 7% annually. In contrast, PCP turnover in the VA system (contract and VA employed) runs as high as 20%. In order to retain the high quality medical providers that veterans deserve, we must materially improve providers’ work-life balance. Requiring providers to spend 77% of a 30-minute appointment doing administrative work and spending seven minutes interacting directly with the veteran is not a sustainable model for provider retention or veteran satisfaction. Additionally, many, many providers are so overwhelmed by the administrative burden inherent with CPRS that they come in early, stay late, or work at home on nights and weekends because they are conscientious medical professionals who want to get their work done. Eventually and inevitably, this sacrifice will not foster a work-life balance that results in long-tenured providers and continuity of care for veterans.
Summary
Access and patient wait times remain a primary challenge for the Veterans Health Administration. While many excellent, effective potential solutions exist, they come with varying costs, risks, and lengthy implementation timelines – all of which delay the healthcare that our nation’s heroes have earned. Meanwhile, the primary care providers charged with caring for veterans have turnover rates 2-3 time higher than the national average. VistA CPRS is a comprehensive electronic health record, but time and the evolution of preventive medicine have burdened both the system and the medical providers who use it with an unsustainable administrative workload that is causing high-quality medical providers to leave the VA healthcare system.
Implementing a medical scribe program in VA Community Based Outpatient Clinics is a single, simple, proven, and budget-neutral solution that can be implemented rapidly for the benefit of veterans and primary care providers alike. Not only does the program increase appointment availability and decrease patient wait times, it reduces medical provider turnover, increases provider retention and delivers the healthcare customer service experience veterans expect, deserve and have earned.
Valor Healthcare can implement our scribe program in any VA Community Based Outpatient Clinic in the country, whether operated by contractor or VA staff, quickly and efficiently. Our management team has over 100 combined years of clinical, operational, and administrative experience in VA healthcare, and we believe VA-private partner collaboration delivers the best practices, best-in-class results veterans deserve in the most time-efficient manner and with a cost-benefit ratio that makes the Veterans Healthcare Administration the most successful integrated healthcare system in the world.
References
i. Understanding the Real Costs of Recruiting and Retaining Physicians. Recruiting Physicians Today, NEJM Career Center. 2012. http://www.nejmcareercenter.org/minisites/rpt/understanding-the-real-costs-of-recruiting/
ii The Health Advocate: A New Concept to Enhance Personalized Pro-Active Health Care. Morgan, et al., 2014. VHA.
iii. Assessment A. Veterans Access, Choice, Accountability Act of 2014. Section 201: Independent Assessment of the Health Care Delivery Systems and Management Processes of the Department of Veterans Affairs. 2014. https://www.va.gov/opa/choiceact/documents/assessments/Assessment_A_Demographics.pdf
iv. Future of Veterans Health Administration’s Home Grown HER Hangs in the Balance. Modern Healthcare. February 2017. http://www.modernhealthcare.com/article/20170210/NEWS/170219989
v. In Search of Joy in Practice: A Report of 23 High-Functioning Primary Care Practices. (Christine Sinsky MD, Willard-Grace MPH, Schutzbank MD, Sinsky MD, Margolius MD, and Bodenheimer MD. 2013. http://www.annfammed.org/content/11/3/272.full
vi. House Veterans Affairs Committee Holds Hearing on Veterans Health Administration Assessment. CQ Congressional Transcripts. October 2015. https://commissiononcare.sites.usa.gov/files/2015/12/20151019-02-HVAC_Hearing_on_Independent_Assessment_CQ-Transcript_7OCT15.pdf
About the Author
Dr. Scott Wise, a U.S. Army veteran, is President of Valor Healthcare, Inc. After leaving the Army in 1998, he was in private practice for 10 years before joining Valor in 2007. He has held successive roles at Valor beginning as a CBOC Medical Director before being named the company’s Chief Medical Officer/Chief of Staff, Chief Operating Officer, and now President. Dr. Wise is Board Certified in Family Medicine.
Valor Healthcare is the largest provider of contract CBOC services to the U.S. Department of Veterans Affairs. Valor serves over 110,000 veterans annually representing a quarter million outpatient primary care visits a year – second only to the VA itself in the delivery of primary care services to America’s veterans.

Scott C. Wise, MD, MBA
President
Valor Healthcare, Inc.






